
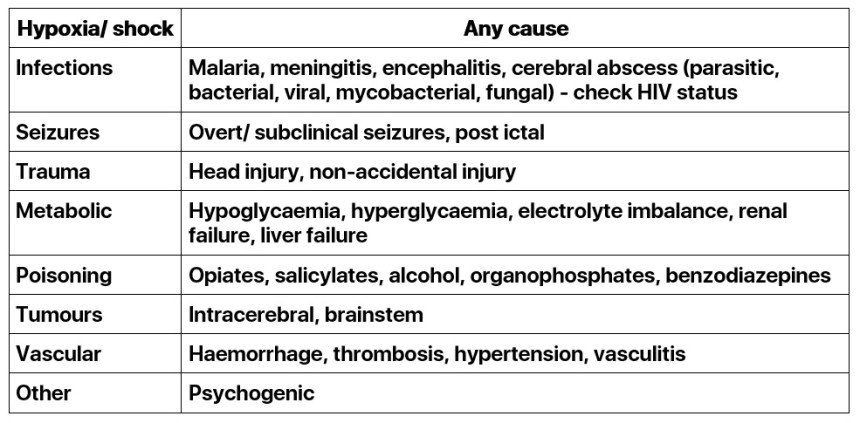
Coma
Common causes
Important points in history
- Timing of onset of coma
- Symptoms of deterioration or recovery
- Fever
- Infants - history of poor or reduced feeding
- History of convulsions
- History of trauma
- History or possibility of dog bite
- Medications in home, including possibility of local mankhwala
- Availability of potential poisons, e.g. organophosphates
- Past medical history, e.g. diabetes, including drug history
- Relevant family history, e.g. diabetes, bleeding diatheses

Important points in examination
AB
Respiratory pattern: may be irregular due to brainstem lesion or raised intracranial pressure. May be rapid due to acidosis or drug ingestion
C
Pulse: Bradycardia suggests raised intracranial pressure or organophosphate poisoning
Blood pressure: Hypertension suggests raised ICP
D
Blantyre coma score (BCS):
Motor: localises (2) withdraws (1) none (0)
Verbal: appropriate cry (2 ) inappropriate (1) none (0)
Eyes: follows (1) does not follow (0)
- Pupil size and reactivity: may reveal signs of drug ingestion, or may be unequal/unreactive due to raised intracranial pressure
- Posture: floppy, extensor posturing, decorticate, decerebrate, opsithotonus
- Fundi: papilloedema (raised ICP), retinal haemorrhages (non-accidental injury)
- Hydration status
- Nutritional assessment
- Pallor
- Oedema: peripheral or facial (renal disease)
- Skin: petechial / purpuric rash (meningococcal disease)
- Breath odour: diabetic ketoacidosis, alcohol ingestion, inborn errors of metabolism
- Neurological examination: to establish a baseline, focal deficits (space occupying
- lesions), lateralising signs (hemiplegia), neck stiffness/ fontanelle (meningitis)
- Gastrointestinal examination: jaundice, splenomegaly (malaria), hepatomegaly (metabolic disorders)
- Trauma: head injury, other injuries
Relevant investigations
- Blood glucose in all patients
- MPS and PCV
- Lumbar puncture:
- if BCS <3 and not post-ictal (even if MPS positive)
- if clinically meningitic or if meningitis cannot be confidently excluded and no contraindications
- Child well enough to tolerate the flexed position
- Cardiovascularly stable, with no signs of bleeding
- No features of raised intracranial pressure
- Blood culture if pyrexial
- Serum electrolytes if available
- Neuroimaging (as dictated by individual case and availability, d/w senior)
- EEG (as dictated by individual case and availability, d/w senior if unsure)
Indications for admission
- All comatose children should be admitted
- If the child has proven meningitis OR has a BCS of 2 or less from any cause, consider admission to the research ward
TreatmentCall for help whenever uncertain
- A Position the airway (using head tilt, jaw thrust, chin lift)
- Consider use of guedel airway
- B Apply oxygen
- C Support circulation in order to maintain normal cerebral perfusion pressure. Treat shock
- Don't ever forget glucose
- If hypoglycaemic, give the child 5ml/kg of 10% dextrose (or 1ml/kg of 50% dextrose), and follow up with regular feeds, or an infusion containing dextrose.
- If no blood sugar test available, assume hypoglycaemia, give 5ml/kg of 10% dextrose (or 1ml/kg of 50% dextrose)
Seizures
- Treat if present Convulsion protocol
Fluids
- Maintain appropriate fluid balance.
- Consider giving 2/3 maintenance (to reduce risk of cerebral oedema), providing no circulatory compromise.
Antimalarials
- Unless there is an obvious cause for the coma (e.g. cloudy CSF indicating meningitis) all comatose children should be given artesunate
Antibiotics
- If clinically meningitic or cloudy CSF give 100mg/kg Ceftriaxone IV/IM daily
Other definitive management
Other treatment will be guided by the history and clinical findings:
- IV Aciclovir if suspension of encephalitis
- Hydralazine /nifedipine if hypertensive encephalopathy
- Atropine if organophosphate poisoning (refer to poisoning protocol)
- Surgical review if trauma suspected (refer to trauma protocol)
Supportive CareNutritional Support
- Unconscious children are often not able to feed, and under NO CIRCUMSTANCES should they be forced: this MUST be explained to the mothers
- Enteral nutrition is preferable: consider insertion of NGT. Can give F100 from Moyo
Other Supportive Care
- Prevent bedsores by turning the patient. Use the recovery position where possible
- Maintain oral hygiene with mouth washes
- Encourage physiotherapy of chest to avoid hypostatic pneumonia, and of limbs to prevent joint contractions
- Nurse at 45 degrees
Monitoring
A comatose child should be monitored at least 4 hourly by a nurse and twice a day by a doctor.
- Pulse
- Respiratory rate
- Temperature
- Blantyre coma score
- Monitor fluids
Blood pressure should be checked if it were previously abnormal or the child has deteriorated
Complications
Acute complications
- Aspiration pneumonia
- Electrolyte imbalance
- Seizures
- Joint contractures
- Secondary septicaemia
Chronic complications
- Cerebral palsy
- Deafness/ visual problems
- Behavioural and learning difficulties
When to Discharge
- When the child has made a full recovery
- After discharge arrange appropriate follow up
- If the child remains static, and after discussion with seniors it is thought unlikely that the child will benefit from any additional inpatient care, and is unlikely to recover further, discuss with the family, and arrange support from Umodzi, physiotherapy, and occupational therapy.





