
Trauma
Causes
- Road traffic accidents: passenger in vehicle (restrained or un-restrained); cyclist vs. vehicle, pedestrian vs. vehicle
- Falls: out of trees, off walls, into septic tanks
- Crush injuries: buildings collapsing
- Burns: electrical, fire, scalds, immersion, lightening
- Drowning: rivers, septic tanks
- Animal bites: dog, snake, hyena, crocodile
- Inflicted injuries: beatings, stabbing, gun shot
Important points in the history
- Age, name
- Date and time of injury
- Mechanism of injury: e.g. road traffic accidents: speed of vehicle, contact point, distance thrown; or fall: height of fall, how landed, what landed on
- If drowning: length of immersion time
- If animal bite: vaccine history
- Events after injury:
- Clinical: loss of consciousness and duration, seizure, vomiting, confusion, abnormal behaviour, bleeding, respiratory arrest
- Treatment given
- Last meal
- Past medical history, social history, family history
- Regular medication, immunisations
- Allergies
- Suspicion of non-accidental injury
Primary survey and emergency managementAirway
- Jaw thrust - avoid "head tilt" in case of cervical spine injuries
- Suction/ removal of foreign body under direct vision (e.g. loose teeth)
- Oxygen via face mask - maximum flow available
- If indicated: guedel airway
- If indicated: intubation & ventilation
Cervical spine protection
- Assume a cervical spine injury in any significant trauma
- In-line immobilisation: using fluid bags and straps (see diagram)
- Rigid collars are NOT used
- If uncooperative/ combative C-spine immobilisation can be harmful
- If significant concern about C-spine injury use log-rolls for position changes, to ensure spine kept in-line

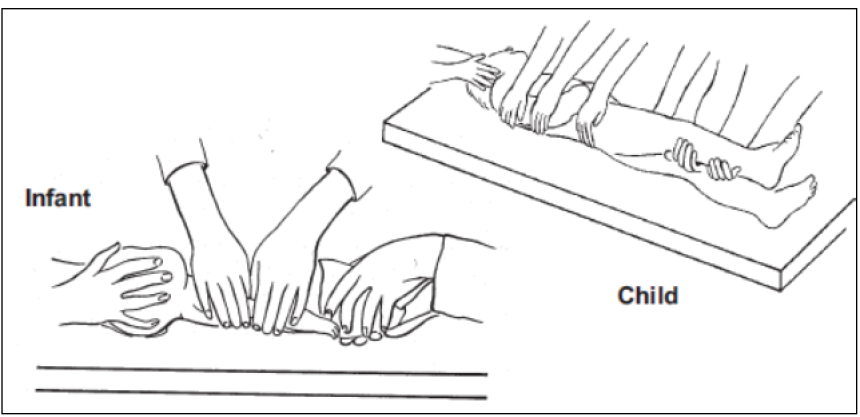
C-Spine immobilisation
- Stabilise the child's neck
- Tape the child's forehead to the sides of a firm board
- Prevent the neck from moving by supporting the child's head e.g. by using bags of IV fluid on each side
- If vomiting use log roll to turn onto one side, keeping the head in line with the body
Breathing
- If respiratory effort is inadequate - start bag mask ventilation
- This child might need intubation and ventilation - Call for HELP!!!
- Check trachea position
- Check chest expansion and check for signs of thoracic injuries
- Tension pneumothorax
- Needle thoracocentesis: 2nd intercostal space, mid-clavicular line, above the rib
- Chest drain insertion will be needed subsequently. Call for HELP!!! While this is being arranged continue with ABC assessment and management
- Haemothorax
- Fluid resuscitation/ transfusion
- Chest drain
- Rib fractures/ flail chest
- Analgesia
- Open thoracic injury (e.g. "sucking chest wound")
- Dressing fixed on three sides
Consider the possibility of cardiac tamponade
- Urgent echo
- Pericardiocentesis if indicated
Consider other mediastinal injuries, disruption of great vessels, diaphragmatic rupture etc.
Indication for intubation and ventilation:
- Persistent airway obstruction
- Predicted airway obstruction (e.g. inhalational burn, severe facial trauma)
- Loss of airway reflexes/ loss of consciousness
- Inadequate respiratory effort or increasing fatigue
- Disrupted ventilator mechanism e.g. flail chest
- Persistent hypoxia despite oxygen administration
- Severe traumatic brain injury
Resources for mechanical ventilation are limited
A pragmatic approach to intubation and ventilation is needed
Call for HELP - experienced paediatrician and/ or anesthetist
Note on the usage of drugs: we use ketamine as an induction agent. In traumatic brain injury the theoretical risk of increasing intracranial pressure is outweighed by the relative haemodynamic stability compared with the use of other induction agents.
Circulation
- Direct pressure to any obvious visible external site of bleeding
- Establish vascular access
- Two 'large' peripheral IV cannulas
- In the event of failure call for HELP
- Intra-osseous cannulation of tibia - avoid injured limb
- External jugular vein, central line (femoral vein etc.)
- Cut down: cephalic vein (elbow)/ long saphenous vein (ankle)
- Sample for cross-match, blood sugar, MPS & PCV
- Assess: HR, central/ peripheral pulses, CRT, temperature gradient +/- pallor, BP (NB: hypotension is a very late sign of severe shock)
- In case of signs of shock/ impaired perfusion
- 10ml/kg ringer lactate or normal saline bolus
- Reassess and repeat fluid bolus if necessary
- If 40ml/kg crystalloids have been administered - use blood transfusion if further fluid boluses are needed.
- Consider type specific or O-negative blood in extreme emergencies
- Contact surgical team early - especially if 20ml/kg do not stabilise the CVS
- Consider thoracic (pneumothorax/ haemothorax), abdominal or pelvic bleeding (bed-side ultrasound scan - FAST scan)
- Blood loss in case of femur fractures can be massive - alignment and traction needed
Disability
- Assess level of consciousness: BCS or AVPU or GCS
- AVPU
- A Alert
- V responds to voice
- P responds to pain
- U unresponsive
- Glasgow coma scale (GCS)

- Pupil size and reactivity to light
- Focal neurology? Bleeding/CSF discharge from ear/nose?
- Urgently contact senior surgeon in case of suspected intracranial haemorrhage
- Discuss if MRI should be done before potential intervention
- Basic management of traumatic brain injury to prevent secondary brain injury:
- Adequate oxygenation
- Control of CO2 tension - (intubation& ventilation might be needed)
- Maintenance of adequate cerebral perfusion pressure (CPP): URGENT correction of shock: inotropes might be needed (ICU only)
- Control of potentially raised ICP: consider mannitol: 250-500mg/kg (1.25 -2.5ml of 20% Mannitol) IV over 30-60 minutes
- Control of hypoglycaemia, convulsions
- Head up position (around 30 degrees)
- Avoid aspiration: insert OGT and keep on free drainage
- Avoid electrolyte imbalance (especially hyponatremia)
- Isotonic fluids or blood for fluid resuscitation
- Use ringer lactate/ normal saline & glucose for maintenance fluids
Exposure
- Examine all parts of the body
- Straighten fractured limbs +/- traction in case of a fractured femur
- Provisional dressings of wounds/ lacerations
Other procedures & imaging
- Emergency imaging if indicated:
- Bedside ultrasound (FAST) scan
- X-rays: skull, lateral C-spine, chest, pelvis, limbs (AP and lateral)
- Patient MUST be stable before being transferred to radiology
- MRI scan brain +/- spine (discuss with consultant)
- Analgesia
- Keep the child warm
- In case of open wounds/ open fractures: tetanus toxoid and antibiotics
Secondary survey after management of ABCDE
- Careful and quick "head to toe examination"
- Reassess ABC & re-examine: thorax, abdomen, pelvis
- Quick neurological exam:
- Level of consciousness, pupils, movements, tone, reflexes
- Fundoscopy if possible
- Check for injuries
- Face & skull - including maxillary/mandibular, dental injuries, check ears, nose, mastoid
- Examine the back of the child. In case of potential spinal injury - the child needs to be "log-rolled" (see diagram)
- Check for injuries/ wounds: skull, neck, thorax, lumbar area, pelvis
- Check spine: in case of suspected acute spinal cord injury - high dose steroids should be started within 8 hours of the injury
Log Roll
- If requesting MRI of brain, also request MRI C-spine
- Keep the head in a neutral position
- Keep the head and body straight, avoid rotation or flexion/extension
- The person holding the head is in charge: hold by placing palms on each side of head, with fingers on the jaw, (do not cover the ears).
- Assistants hold the arms and legs (see below) to keep the body in line.
- On the instructions of the lead person turn the patient onto their side to allow the back to be examined, or the patient to vomit
- Guidelines for clearing a cervical spine
- Remember- despite normal x-rays the child can have a spinal cord injury without radiological abnormalities (e.g. haematomas, ligament injuries) - SCIWORA
- The child should be cooperative and alert
- No midline cervical tenderness on direct palpation
- No focal neurological deficit
- No painful distracting injuries
- Examination of limbs - signs of fractures?
- In case of severely angulated fractures - alignment and splinting +/- traction
- Any signs of open fractures?
- In this case tetanus toxoid and IV antibiotics needed
- Any deep wound within vicinity of a fracture could communicate with fracture
- Any signs of compartment syndrome? Monitor perfusion and pulses
- Any signs of vascular injury? Check perfusion and pulses
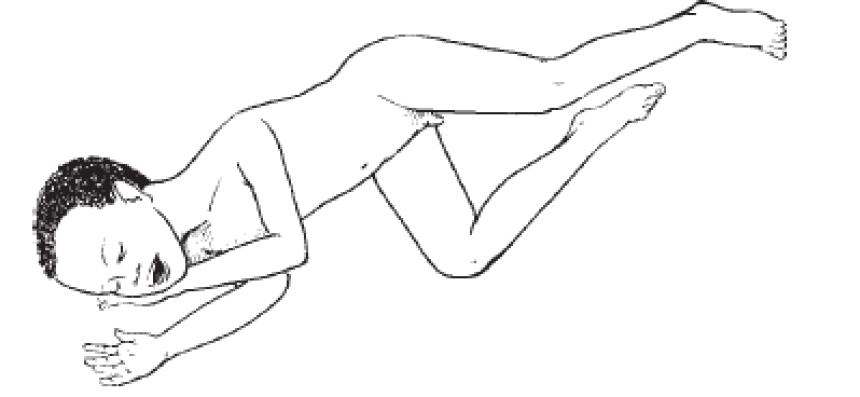
How to position the unconscious child
No Neck Trauma: Recovery Position
Turn the child on to their side to reduce the risk of aspiration
Keep the neck slightly extended and stabilise by placing the cheek on one hand
Bend one leg to stabilise the body position
Transfer & further management
- Reassess ABCDE regularly
- Ensure adequate analgesia
- Transfer to HDU, theatre, ICU, radiology department
- Critically ill children need to be accompanied by nurse +/- doctor
- Take resuscitation equipment with you
- Use oxygen cylinder for transfer of sick children
- Handover to receiving team
- Regular monitoring on HDU, including "neuro-observations" in severely injured child
- Signs of raised ICP due to cerebral oedema or intracranial haematomas (e.g. extradural) can present even hours after initial presentation
- Encourage parents to alert nurses or medical team in case of any concern





