
Admin Name
10 months ago
admin
#haematology
Anaemia
For FFP and platelets see Bleeding protocol, section treatment.
 Transfusion Requirement
Transfusion Requirement- Hb < 4 g/dL ~ PCV < 12%
- Hb < 6 g/dL ~ PCV < 18% AND:
- Dehydration
- Shock
- Significant respiratory distress or acidosis
- Prostration (inability to sit up)
- Heart Failure
- MPS 4+
- BCS less than or equal to 3
(most common causes written in CAPITALS - always check and treat those in Malawi as their presence significantly increases post-discharge mortality)
 Important points in history
Important points in history- Bleeding (tendency) (nose/ gums/ stool/ urine)
- Jaundice
- Colour of urine
- Fever
- Previous transfusions
- History of painful crises (SCD)
- Drug history (G6PD)
- Family, social and geographic history
- Respiratory
- Rate/Pattern
- Heart rate/ Cardiac failure
- BCS
- Jaundice
- Malnourished
- Dehydrated
- Septic/ Shocked
- Enlarged Nodes/ Spleen/ Swellings
- Bleeding/ haematoma/ trauma
- Bone deformities/ frontal bossing
- In all children check:
- MPs + PCV + HIV status
- Grouping and Cross-match if transfusion is being considered
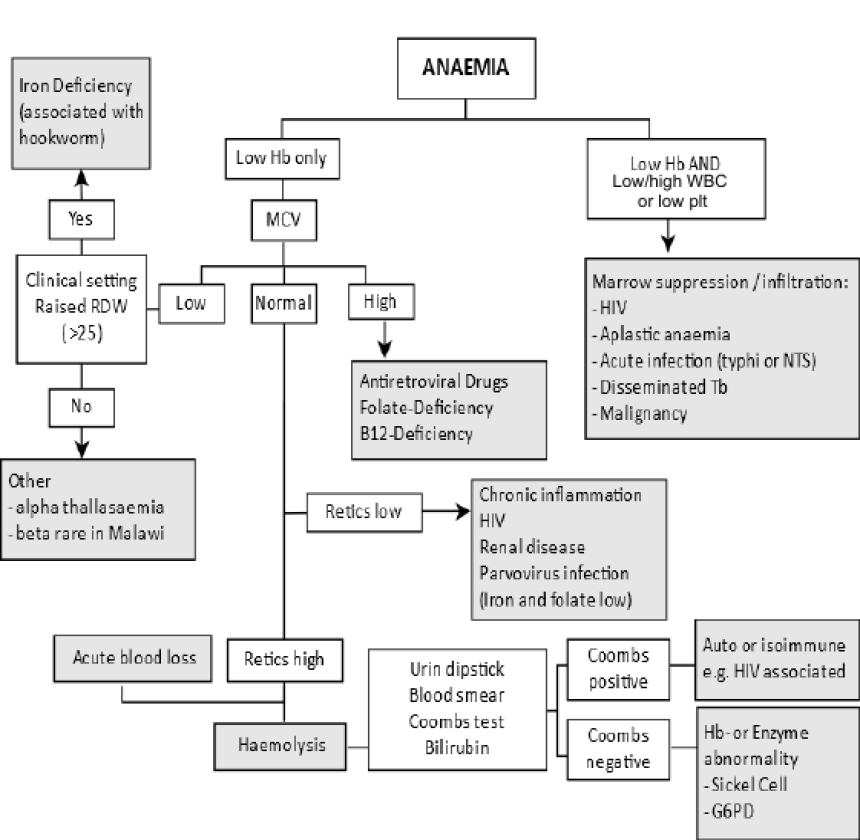
- If the MPS are negative or if other disease suspected:
- Full Blood Count (look at MCV) + Diff. - take BEFORE transfusion
- Blood Culture if septicaemia considered
- If signs of other disease present consider:
- Urinalysis
- Sickle Cell test
- Chest X-Ray
- Stool for parasites and/or occult blood
- Peripheral blood film (to exclude malignancy) - send to department lab
- Consider Bone Marrow Biopsy after FBC results discussed
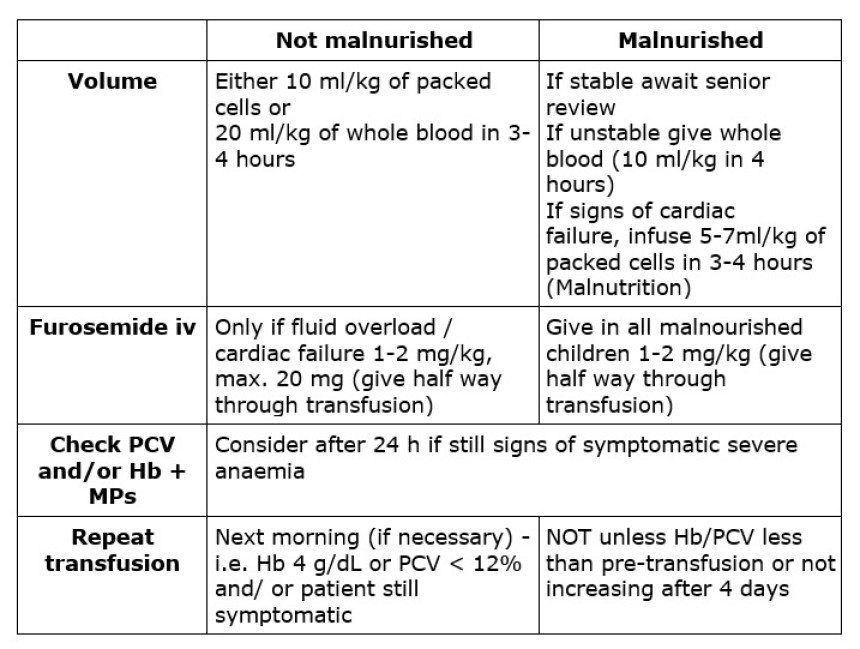
- Blood transfusion (Indicate volume and PCV result on the requesting form), deliver the sample to blood bank, follow up to obtain the crossmatched blood
- Oxygen - even with good saturations (will improve O2 delivery to tissues)
- Treat cause (e.g. Artesunate, antibiotics, antihelminths etc)
- Persistent fever after 48 hrs of Artesunate: consider Salmonella infection
 Discharge and follow-up
Discharge and follow-up- Discharge when child is pink (Hb > 4 g/dL or PCV > 12% and asymptomatic), not vomiting, no oedema
- Albendazole treatment to ALL anaemic children > 1 year
- Ferrous sulfate and folic acid to all anaemic children except those with sickle cell disease (DO NOT GIVE IRON SUPPLEMENTS TO A CHILD WITH ACUTE MALARIA/ SEPTICAEMIA. WAIT UNTILL THEY ARE DISCHARGED.) FeFol will be needed for 3 months
- Check that children have a bed net at home. If not, give one from A&E
- Arrange a health centre follow-up 2 weeks after discharge for PCV/ Hb (there is a high risk of recurrence/ death in the first month after transfusion)





