Triage
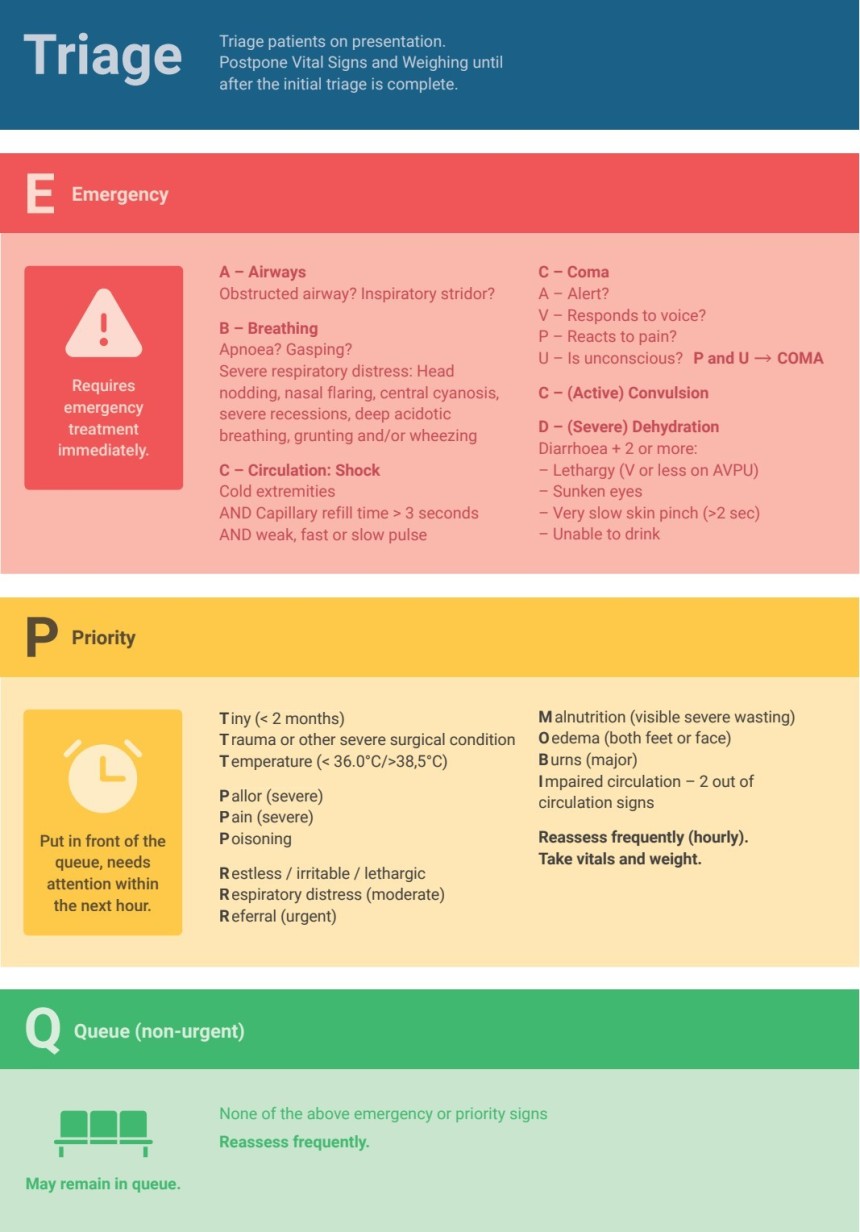
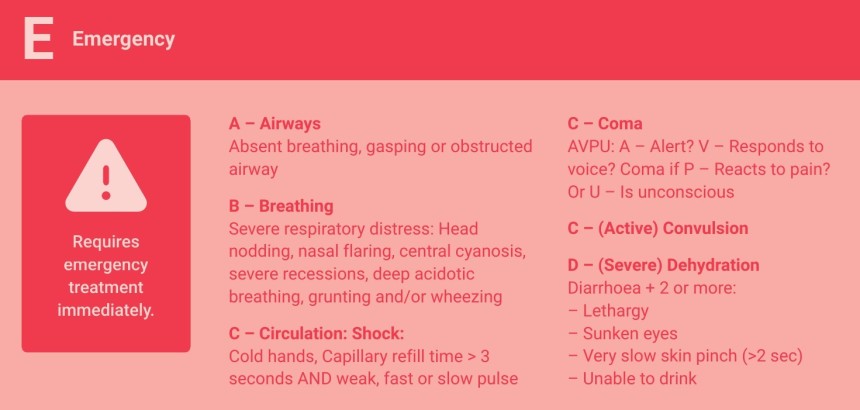
Triage is the process of identifying signs of serious illness or injury in patients and categorizing them based on the urgency of care needed. The key emergency signs to look for—Airway, Breathing, Circulation, Coma, Convulsions and Severe Dehydration—can be easily remembered using the acronym ABCCCD:
· A − Airway obstruction
· B − Breathing difficulties
· C − Circulation issues (shock, severe anemia)
· C − Coma (unresponsiveness)
· C − Convulsions (seizures)
· D − (Severe) Dehydration
Each of these signs indicates a life-threatening condition requiring immediate assessment and intervention. Early recognition is essential for improving patient outcomes.
The Triage Process
Triage must be performed immediately when a child arrives at the hospital before any administrative procedures like registration. The goal is to quickly differentiate stable children from those needing urgent care and prioritize treatment accordingly.
Triage Categories
Children are classified into three groups based on the severity of their condition:
1. Emergency Cases − Children with life-threatening conditions requiring immediate intervention.
2. Priority Cases − Children with priority signs who need prompt assessment and treatment to prevent deterioration.
3. Non-Urgent Cases − Children without emergency or priority signs who can safely wait for their turn in the queue for routine assessment and treatment. Most sick children fall into this category.
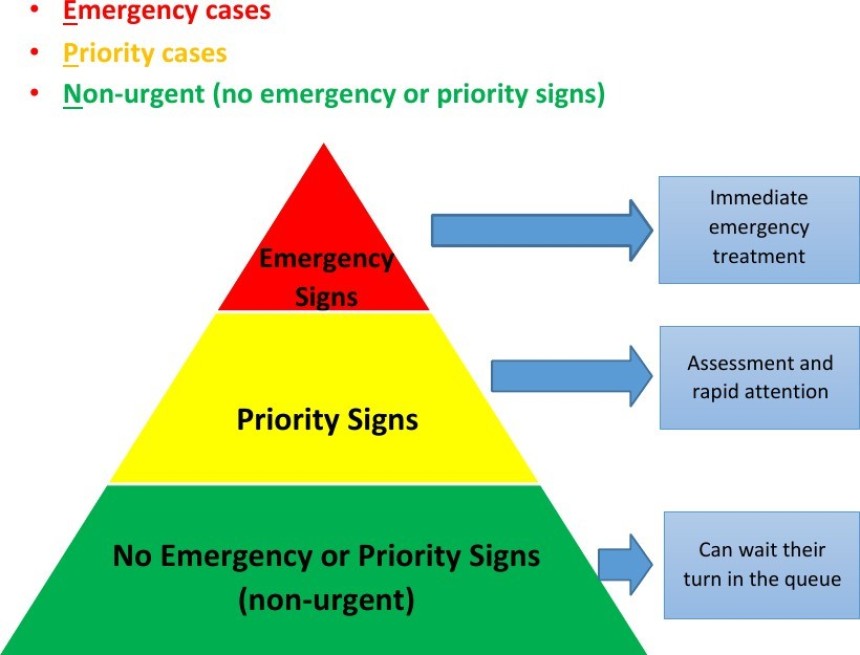
Check for emergency signs. If present, the child must be immediately transferred to the emergency area for life−saving treatment. Triage stops at this point, and there is no need to continue the assessment, measure vital signs, or record weight.
If no emergency signs are found, assess for priority signs. This should take only a few seconds. Children with priority signs should be moved to the front of the queue, and a clinician should be notified.
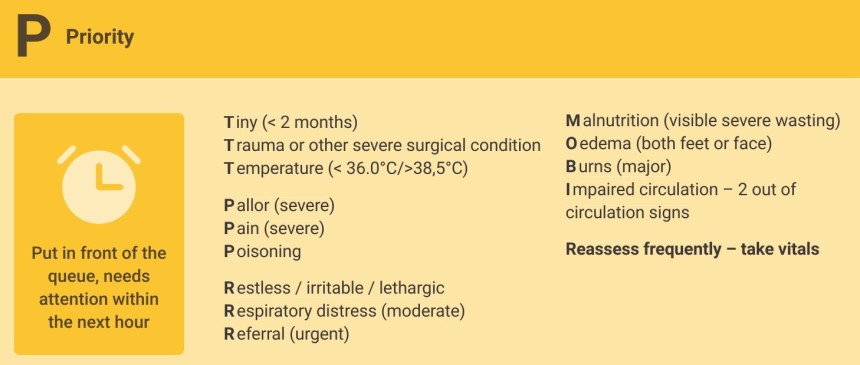
Additional information on the assessment of priority signs:
· T iny − neonates and infants less than 2 months
· T rauma or other severe surgical condition − fall from height, road traffic accidents, acute abdominal pain, acute inguinal hernias and many more
· T emperature (<36.0˚C/>38.5˚C) on measurement of vital signs
P allor (severe) − severely pale palms of hands and feet (compare with your own and caretaker’s palms)
· P ain (severe) − especially if sickle cell disease patient
· P oisoning − history of taking drugs, ingestion of soda powder etc., also snake bites
· R eferral (urgent) − urgent referral letter
M alnutrition − visible severe wasting. Hanging axillar skin folds, baggy pants buttocks, bony rib cage, thin arms and legs, granny face
· O edema (feet or face)
· B urns (major) − >10% of body surface area (palm of patient equals to 1%), involvement of genitalia, facial burn, circumferential burns
· I mpaired circulation − 2 out of the 3 circulation signs (cold extremities, prolonged capillary refill time >3 sec, weak and fast pulse)
If neither emergency nor priority signs are present, the child is classified as non-urgent and can wait in the queue for routine assessment and treatment.
Re-Triage: If a child’s condition worsens while waiting, they must be re-triaged immediately
to ensure they receive timely care.
Triage Summary